Supplemental Reviews
Wondering if there is money left on the table after initial or additional reviews? Apogee conducts subsidiary reviews for accounts previously reviewed and provides detailed analysis on prior performance as well as collecting any underpaid accounts that may arise after a second look.
Making certain that organizations receive the utmost maximum reimbursement is a must in today's healthcare industry. There is always room for improvement, even at 99% collectability. At an all-inclusive contingency fee, supplemental reviews are a win-win for all providers.
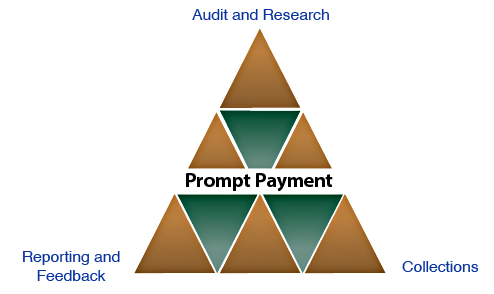

Audit & Research
Using both proprietary software and manual reviews, Apogee performs a detailed analysis of all previously reviewed inpatient and outpatient zero insurance balance accounts. Research on the claims is conducted to revalidate correct reimbursement calculation as well as gathering claim information to confirm all insurance payments owed are received.

Collections
If Apogee identifies underpaid claims during the course of our audit, our professional staff contacts payers and diligently follows up on each claim until the issue is resolved and revenue is recovered.

Reporting & Feedback
Apogee unites with its clients to certify all expectations are met by previous reviews. This is achieved through periodic detailed reports presented to management and regular feedback to maximize cash flow and decrease account receivable days. Apogee provides specific feedback as it relates to underpayment issues for each payer.
