Managed Care Services
In today's complex healthcare environment, ensuring proper reimbursement from all payers can be very challenging. With over 90% of all revenue in healthcare today coming from insurance payers (Medicare, Medicaid, and Commercial payers), it is crucial providers review all reimbursement accurately.
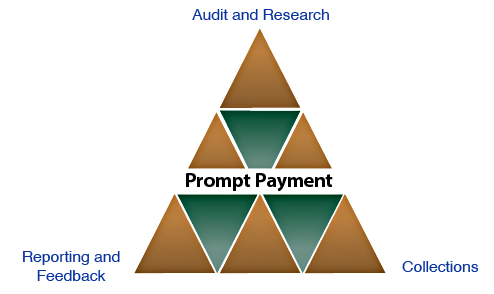

Audit & Collections
Apogee performs a detailed analysis of all zero insurance balance inpatient and outpatient accounts for all payers and plans using proprietary software and manual review. Our professional staff contacts payers and diligently pursues each claim until the issue is resolved and revenue is recovered.

Contract Negotiations
Apogee researches and reviews market and contractual terms for increased reimbursement. Apogee's national presence allows for a comprehensive review of underpayment trends by insurance companies. Providing clients with feedback on issues such as contract language and payment terms greatly increases reimbursement and decreases underpayments. Our experience and attention to detail result in higher reimbursement from managed care payers.

Reporting & Education
Apogee partners with clients to ensure all expectations are met. This is achieved by periodic detailed reports to the client's management staff. Apogee provides detailed findings and recommendations to minimize recurring issues during onsite progress reports. However, underpayment resolution cannot be corrected with reports and feedback alone. As part of our contingency fee, we provide development and training for staff members. Apogee provides educational seminars explaining reasons for underpayments and how to resolve issues internally specific to the organization.
