Prompt Payment Reviews
With changes in healthcare upon us, timely payment on claims is a necessity for providers across the nation to meet their financial needs for future growth and profitability.
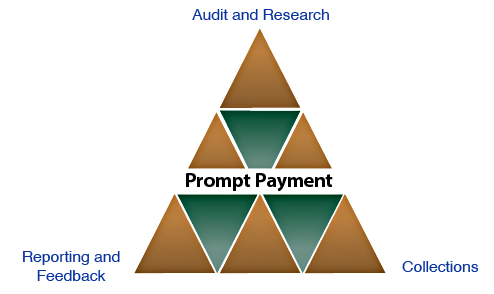

Audit & Research
Apogee audits and researches each claim for untimely payments according to contractual obligations or legislative statutes. Finding a claim eligible for penalties can be like that needle in a haystack, you know it's there, but where? There are several steps to confirm if penalties are due which may consume an ample amount of your staff's valuable time. Apogee's comprehensive review of payment history, request of information, plan eligibility, and proper billing will confirm whether claims are entitled to prompt payment penalties.

Collections
After verifying clean claim required elements, plan eligibility, and valid untimely payment history, Apogee initiates the collection process. Our professional staff contacts payers and routinely follows-up on each claim until the penalty is recovered.

Reporting & Feedback
In-depth information of our results is an imperative part of ensuring increased efficiency in timely payments for clients. This is achieved through periodic detailed reports presented to management and regular feedback to maximize penalty recovery and decrease account receivable days. Apogee provides specific feedback as it relates to each payer and issues associated with untimely payment.
